This “Powerful Components Of Cardiac Rehabilitation Programs” article is exploring about the key steps for better restoration in Cardiac rehabilitation (CR) because this a crucial intervention for individuals recovering from heart disease or undergoing cardiac procedures. Among the various components of CR, exercise training plays a pivotal role in promoting recovery, improving cardiovascular health, and enhancing overall quality of life. This “Powerful Components Of Cardiac Rehabilitation Programs” article delves into the multifaceted benefits of exercise training in cardiac rehabilitation, the types of exercises recommended, and the underlying mechanisms that contribute to its efficacy.
Understanding Components Of Cardiac Rehabilitation
Cardiac rehabilitation is a comprehensive program designed for individuals with heart conditions, including those who have experienced heart attacks, undergone heart surgery, or have chronic heart diseases. The program typically includes:
- Medical evaluation
- Supervised exercise training
- Nutritional counseling
- Psychological support
- Education on heart health
Importance of Exercise Training in Cardiac Rehabilitation
Exercise training is a fundamental aspect of CR, as it provides numerous physical, psychological, and social benefits. Engaging in a structured exercise program helps patients regain strength, improve their cardiovascular fitness, and promote healthier lifestyles.
Benefits of Exercise Training in Cardiac Rehabilitation
1. Enhancing Cardiovascular Fitness
One of the primary goals of exercise training is to improve cardiovascular fitness. Regular physical activity strengthens the heart muscle, enabling it to pump blood more efficiently. This improved efficiency can lead to lower resting heart rates and enhanced exercise tolerance.
Research Evidence
Studies indicate that patients who participate in exercise training during CR experience significant improvements in their peak oxygen uptake (VO2 max), a key indicator of cardiovascular fitness. For instance, a meta-analysis published in the Journal of the American College of Cardiology found that exercise training increased VO2 max by approximately 15% in cardiac rehabilitation patients (Piepoli et al., 2016).
2. Managing Risk Factors
Exercise training plays a vital role in managing risk factors associated with heart disease, such as hypertension, hyperlipidemia, and obesity.
A. Blood Pressure Control
Regular aerobic exercise has been shown to lower blood pressure in hypertensive patients. A study in the American Journal of Hypertension reported that individuals who engaged in regular aerobic exercise saw a reduction in both systolic and diastolic blood pressure levels (Cornelissen & Fagard, 2005).
B. Cholesterol Management
Exercise can positively affect lipid profiles, helping to lower LDL (bad cholesterol) and increase HDL (good cholesterol). This is particularly important for individuals with a history of heart disease, as maintaining healthy cholesterol levels can significantly reduce the risk of future cardiovascular events.
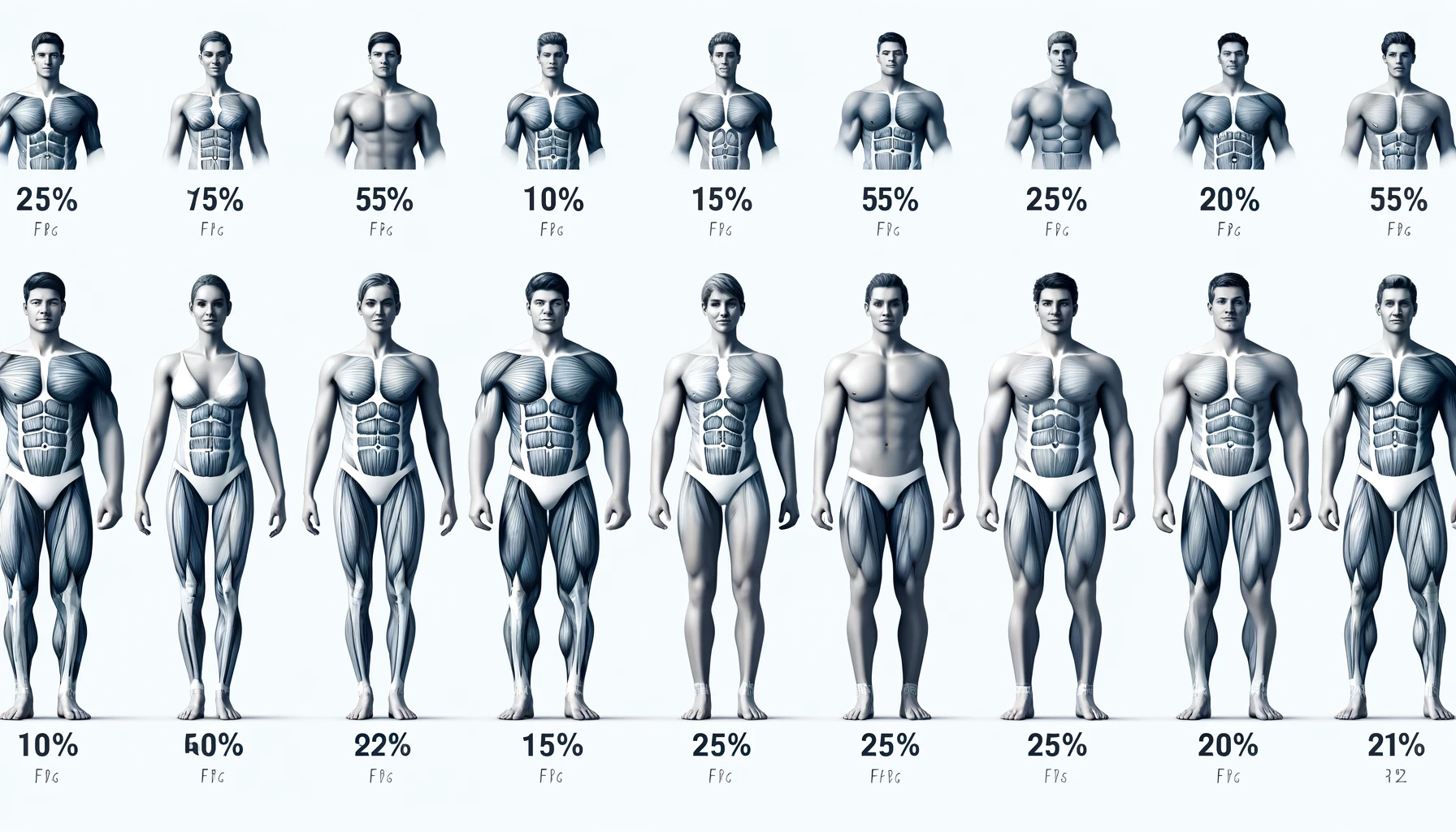
3. Weight Management
Obesity is a major risk factor for heart disease. Exercise training, combined with dietary changes, can facilitate weight loss, and help individuals achieve a healthier body weight. This, in turn, contributes to improved cardiovascular health.
4. Improving Psychological Well-Being
Cardiac events can lead to anxiety and depression. Exercise training has been shown to improve mood and reduce symptoms of anxiety and depression in individuals undergoing cardiac rehabilitation.
Psychological Benefits
- Endorphin Release: Exercise stimulates the release of endorphins, which are natural mood lifters.
- Social Interaction: Group exercise sessions foster social connections, further enhancing emotional well-being.
5. Enhancing Functional Capacity
Exercise training improves the functional capacity of individuals, enabling them to perform daily activities with greater ease and less fatigue. This increased endurance can lead to improved overall quality of life.
6. Reducing Hospitalization Rates
Research indicates that patients who participate in structured exercise training during CR have lower rates of hospitalization due to cardiovascular events. A study published in Circulation found that comprehensive CR, including exercise training, led to a 20-30% reduction in mortality rates among participants (Gonzalez et al., 2018).
Components of Cardiac Rehabilitation: Exercise Training
1. Aerobic Exercise
Aerobic exercises, such as walking, cycling, and swimming, are the cornerstone of exercise training in CR. These activities elevate the heart rate and improve cardiovascular endurance.
- Recommended Frequency: At least 150 minutes of moderate-intensity aerobic activity per week, or 75 minutes of vigorous-intensity activity.
- Examples: Brisk walking, cycling on a stationary bike, or swimming.
2. Resistance Training
Incorporating resistance training into CR can help patients build muscle strength and endurance.
- Recommended Frequency: At least two days per week, focusing on major muscle groups.
- Examples: Using free weights, resistance bands, or weight machines.
3. Flexibility and Balance Training
Flexibility and balance exercises are essential for improving overall mobility and preventing falls, especially in older adults.
- Recommended Frequency: At least two to three days per week.
- Examples: Stretching exercises, yoga, or tai chi.
Implementing Exercise Training in Cardiac Rehabilitation
1. Supervised Programs
Most CR programs offer supervised exercise training, where healthcare professionals to ensure safety and adherence monitor patients. This supervision is crucial for patients with significant comorbidity or those who are new to exercise.
2. Personalized Exercise Plans
Exercise training should be tailored to each patient’s individual needs, preferences, and limitations. A thorough assessment by healthcare providers can help determine appropriate exercise intensity, duration, and frequency.
3. Self-Monitoring and Progress Tracking
Encouraging patients to self-monitor their exercise progress can enhance motivation and adherence. Tools such as fitness trackers or mobile applications can be helpful for tracking activity levels and setting achievable goals.
Creating a safe and effective exercise program for a 50-year-old individual who has recently recovered from angina pectoris is crucial for promoting cardiovascular health. The following 7-day exercise program emphasizes gradual progression, incorporating aerobic, strength, and flexibility exercises. Always consult a healthcare provider before starting any new exercise regimen.
7-Day Exercise Program: Essential Components of Cardiac Rehabilitation
Day 1: Aerobic Activity
- Warm-Up: 5-10 minutes of gentle stretching or walking at a slow pace.
- Main Exercise:
- Walking: 20 minutes at a moderate pace (aim for a pace where talking is possible but requires some effort).
- Cool Down: 5-10 minutes of slow walking followed by stretching.
Day 2: Strength Training
- Warm-Up: 5-10 minutes of light walking.
- Exercises:
- Body weight Squats: 2 sets of 8-10 reps
- Seated Leg Lifts (while seated): 2 sets of 10 reps per leg
- Wall Push-Ups: 2 sets of 8-10 reps
- Dumbbell Curls (light weights, if cleared by a doctor): 2 sets of 8-10 reps
- Cool Down: 5-10 minutes of stretching, focusing on major muscle groups.
Day 3: Flexibility and Balance
- Warm-Up: 5-10 minutes of gentle walking.
- Exercises:
- Static Stretching: Hold each stretch for 15-30 seconds (focus on arms, legs, and back).
- Yoga or Tai Chi: 20-30 minutes focusing on deep breathing and gentle movements.
- Cool Down: Continue stretching.
Day 4: Aerobic Activity
- Warm-Up: 5-10 minutes of gentle stretching or walking.
- Main Exercise:
- Cycling (stationary bike): 20 minutes at a comfortable pace.
- Cool Down: 5-10 minutes of slow cycling or walking followed by stretching.
Day 5: Strength Training
- Warm-Up: 5-10 minutes of light walking.
- Exercises:
- Seated Row (using resistance bands): 2 sets of 8-10 reps
- Step-Ups (onto a low step): 2 sets of 8-10 reps per leg
- Standing Calf Raises: 2 sets of 10 reps
- Shoulder Press (with light weights): 2 sets of 8-10 reps
- Cool Down: 5-10 minutes of stretching.
Day 6: Aerobic Activity
- Warm-Up: 5-10 minutes of gentle stretching or walking.
- Main Exercise:
- Brisk Walking: 25 minutes, slightly increasing pace from Day 1.
- Cool Down: 5-10 minutes of slow walking followed by stretching.
Day 7: Rest and Recovery
- Activity: Engage in light activities like walking or gardening for 20-30 minutes, if comfortable.
- Focus: Take this day to rest, hydrate, and reflect on the week’s progress.
Important Considerations:
- Monitor Symptoms: Pay attention to any signs of discomfort or unusual symptoms during exercise, such as chest pain, shortness of breath, or dizziness.
- Hydration: Stay hydrated before, during, and after workouts.
- Intensity: Maintain a moderate intensity level. A good guideline is the “talk test” — if you can talk but not sing, you’re likely at a moderate intensity.
- Consultation: Regular follow-up with a healthcare provider or cardiac rehabilitation specialist is essential for ongoing evaluation and adjustments to the exercise program.
This exercise program serves as a starting point for safely reintroducing physical activity. Adjustments can be made based on individual progress and comfort levels.
“Cardiac Rehabilitation Programs: Final Thoughts”
The role of exercise training in cardiac rehabilitation cannot be overstated. It not only enhances cardiovascular fitness and helps manage risk factors but also improves psychological well-being and overall quality of life. With personalized exercise plans and supervised training, individuals recovering from heart conditions can regain their strength, reduce the risk of future events, and lead healthier lives.
Frequently Asked Questions (FAQs)
- What is cardiac rehabilitation? Cardiac rehabilitation is a structured program designed to help individuals recover from heart disease through exercise, education, and support.
- How long does a cardiac rehabilitation program typically last? Most programs last between 12 to 36 weeks, depending on individual needs.
- What types of exercises are included in cardiac rehabilitation? Aerobic exercises, resistance training, and flexibility exercises are commonly included.
- Is exercise safe for all cardiac patients? While exercise is beneficial, patients should always consult their healthcare provider to determine safe levels of activity.
- How does exercise improve heart health? Exercise strengthens the heart muscle, improves blood circulation, and helps manage risk factors like blood pressure and cholesterol.
- Can exercise training reduce the risk of future heart events? Yes, studies have shown that regular exercise can significantly lower the risk of future cardiovascular events.
- What should I expect during a cardiac rehabilitation program? Participants can expect medical evaluations, supervised exercise sessions, nutritional counseling, and education on heart health.
- Are there psychological benefits to exercise in cardiac rehabilitation? Yes, exercise can reduce anxiety and depression and enhance overall mood.
- Can family members participate in cardiac rehabilitation? Many programs encourage family involvement to support the patient’s recovery process.
- How can I find a cardiac rehabilitation program near me? Consult your healthcare provider or search online for accredited cardiac rehabilitation programs in your area.
References
- Piepoli, M. F., et al. (2016). “Exercise training in cardiac rehabilitation: A systematic review and meta-analysis.” Journal of the American College of Cardiology.
- Cornelissen, V. A., & Fagard, R. H. (2005). “Effects of exercise on blood pressure control in hypertensive patients: A meta-analysis.” American Journal of Hypertension.
- Gonzalez, A. L., et al. (2018). “Cardiac rehabilitation and mortality: A systematic review and meta-analysis.” Circulation.
- American Heart Association. (n.d.). “Cardiac Rehabilitation.” American Heart Association.
For additional information and resources related to cardiac health, consider visiting reputable organizations like the American Heart Association or Mayo Clinic