The Medial Collateral Ligament, or MCL, is a crucial ligament that stabilizes the knee joint and allows for fluid, controlled movement. Located on the inner side of the knee, the MCL connects the thighbone (femur) to the shinbone (tibia), creating a vital support system for the knee. Injuries to this ligament can occur during various physical activities, especially sports that involve sudden changes in direction or impact to the knee. Understanding the causes, symptoms, and treatment options for an MCL injury is essential for anyone affected by or at risk of this common knee injury.

Anatomy of the Medial Collateral Ligament
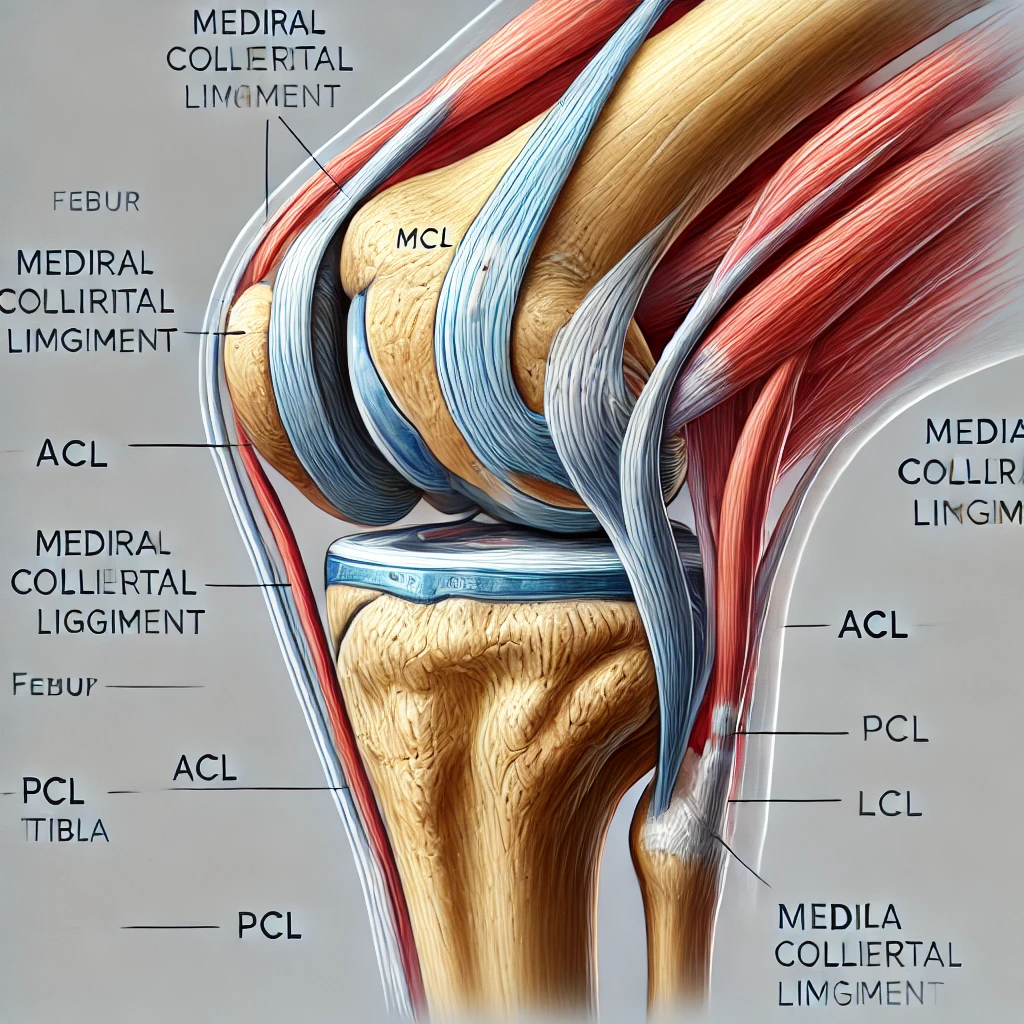
The MCL is a thick, broad band of fibrous tissue running along the inside of the knee joint. Its primary role is to prevent the knee from bending inward excessively, stabilizing the joint under physical stress. The MCL is part of a group of four main ligaments in the knee, including the Anterior Cruciate Ligament (ACL), Posterior Cruciate Ligament (PCL), and the Lateral Collateral Ligament (LCL), each contributing to overall knee stability. Together, they work to protect the knee from unwanted or excessive motion, with the MCL specifically resisting forces that would otherwise push the knee inward.
Causes of Medial Collateral Ligament Injuries
Medial Collateral Ligament injuries typically result from a force that pushes the knee inward, stretching, or tearing the ligament. These forces are commonly encountered in sports like football, soccer, and skiing, where athletes frequently change direction, pivot, or experience collisions. Additionally, accidents like slipping on wet surfaces or sudden falls can put unexpected pressure on the knee, leading to an MCL injury. Factors that increase the likelihood of MCL injury include poor conditioning, lack of flexibility, and inadequate warm-up before physical activities.
Types of Medial Collateral Ligament Injuries
Medial Collateral Ligament injuries are categorized into three grades based on severity:
- Grade 1: A mild sprain where the ligament is stretched but not torn. It usually causes slight pain and tenderness but doesn’t result in significant instability.
- Grade 2: A partial tear in the ligament, leading to moderate pain and noticeable swelling. Knee stability is moderately affected.
- Grade 3: A complete tear of the MCL, resulting in severe pain, swelling, and an unstable knee that may feel like it “gives way” under pressure.
Understanding the injury grade is essential for determining the appropriate treatment and recovery plan.
Symptoms of Medial Collateral Ligament Injury
An MCL injury manifests through various symptoms, with pain being the most immediate. This pain is typically felt on the inner side of the knee, increasing during movement or when pressure is applied. Other symptoms include:
- Swelling and Bruising: Often appearing within a few hours post-injury, the knee may swell and exhibit bruising due to blood pooling.
- Instability: A torn MCL may cause the knee to feel unstable or as though it may buckle under weight.
- Restricted Movement: The injury may limit the knee’s range of motion, making activities like walking and climbing stairs painful.
Diagnosing an Medial Collateral Ligament Injury
Proper diagnosis is crucial for effective treatment. A healthcare provider will often begin with a physical examination, testing the knee’s stability by applying gentle pressure. They may ask the patient to move the knee in various directions to identify painful or restricted motions. To confirm the extent of the injury, imaging tests like X-rays (to rule out bone fractures), MRI (to assess soft tissue damage), and ultrasound (to examine ligament health) are commonly used. An accurate diagnosis ensures a tailored treatment plan based on the severity of the injury.
Immediate First Aid for Medial Collateral Ligament Injury
If an MCL injury is suspected, immediate action can prevent further damage. The RICE method (Rest, Ice, Compression, Elevation) is the first step:
- Rest: Limit movement and avoid weight-bearing activities to prevent worsening the injury.
- Ice: Applying ice packs every few hours reduces swelling and numbs the pain.
- Compression: Wrapping the knee with an elastic bandage minimizes swelling and provides light support.
- Elevation: Raising the leg helps reduce fluid buildup and swelling.
In addition, a knee brace can provide stability, helping to reduce pain and movement. However, it’s essential to consult a medical professional for further evaluation, especially if the pain persists.
Non-Surgical Treatment Options
For most MCL injuries, especially Grades 1 and 2, non-surgical treatments are effective. These treatments include:
- Physical Therapy: Guided exercises help strengthen the surrounding muscles and restore knee function, particularly targeting flexibility and stability.
- Medications: Over-the-counter anti-inflammatory medications like ibuprofen help manage pain and reduce inflammation.
- Bracing: Using a knee brace or support stabilizes the knee during the recovery phase, especially beneficial during physical therapy sessions or light daily activities.
Adhering to a prescribed treatment plan ensures a faster, more effective recovery and reduces the risk of re-injury.
Surgical Treatment for Severe Medial Collateral Ligament Tears
In cases of a Grade 3 MCL injury, or if the tear doesn’t respond to non-surgical methods, surgery may be considered. Surgery generally involves reconstructing or reattaching the torn ligament, often through minimally invasive techniques. The choice of surgical method depends on the injury’s complexity and may involve tissue grafts or synthetic materials to support healing. After surgery, physical therapy is essential to rebuild strength and restore knee mobility, with a recovery timeline that can span several months.
Rehabilitation and Physical Therapy
Rehabilitation is essential for restoring full knee functionality. A physical therapist will tailor exercises to increase strength, flexibility, and range of motion in the knee. Common rehabilitation exercises include:
- Quadriceps strengthening: Exercises like leg raises to build thigh strength
- Range of motion exercises: Gentle stretches and movements to improve knee flexibility
- Balance training: Helps regain knee stability and reduces the risk of future injuries
Rehabilitation ensures a comprehensive recovery by addressing both the injured ligament and overall knee stability.
Recovery Timeline for Medial Collateral Ligament Injuries
The recovery time for an MCL injury varies based on the severity and the chosen treatment approach. Here’s a general timeline for each grade:
- Grade 1 (Mild Sprain): Recovery typically takes 1-2 weeks. During this time, rest and gentle movement are crucial, and physical therapy may help speed recovery.
- Grade 2 (Partial Tear): With a partial tear, recovery can take 3-4 weeks. This period involves a combination of rest, physical therapy, and possibly the use of a knee brace.
- Grade 3 (Complete Tear): Recovery from a complete tear can extend up to 8-12 weeks, especially if surgery is required. After surgical intervention, rehabilitation is vital to regain strength and stability.
Factors such as age, physical fitness, and adherence to the rehabilitation plan influence the recovery timeline. A focus on consistent rehabilitation exercises and rest can significantly improve healing and reduce long-term complications.
Potential Complications and Long-term Effects
While many individuals recover fully from MCL injuries, some may experience complications if proper treatment isn’t followed. Potential issues include:
- Chronic Knee Instability: Insufficient rehabilitation or untreated tears can lead to a “loose” knee feeling, making it prone to future injuries.
- Arthritis Development: A history of knee injuries, particularly ligament tears, increases the risk of arthritis in the knee joint as a long-term complication.
- Reduced Range of Motion: Scar tissue or improper healing can limit knee flexibility, making activities like running, squatting, or even walking uncomfortable.
Managing these risks involves consistent follow-up care, adherence to rehabilitation exercises, and regular check-ups to monitor knee health.
Preventing Medial Collateral Ligament Injuries
Taking proactive steps to protect the MCL can prevent injuries, especially for athletes and those with active lifestyles. Here are some key prevention strategies:
- Warm-Up Exercises: Engaging in warm-up routines, especially for the lower body, preps the muscles and ligaments, reducing the risk of strain or tears.
- Strength Training: Strengthening the muscles around the knee, such as the quadriceps, hamstrings, and calf muscles, provides additional support to the MCL.
- Proper Technique in Sports: Learning and practicing correct techniques for jumping, landing, and changing direction reduces stress on the knee and minimizes the risk of injury.
- Protective Gear: Using knee braces or supports in high-impact sports can protect the knee from sudden movements or impacts.
By incorporating these practices, individuals can maintain knee stability and reduce the likelihood of sustaining an MCL injury.
Living with Medial Collateral Ligament Injury: Tips and Coping Mechanisms
Living with an Medial Collateral Ligament injury, even temporarily, can impact daily life. Here are some strategies for managing day-to-day activities and reducing discomfort:
- Modify Physical Activities: While healing, it’s wise to avoid high-impact activities. Opt for gentle exercises like walking, swimming, or cycling to stay active without putting stress on the knee.
- Use Supportive Aids: Knee braces, crutches, or even walking aids can reduce pressure on the knee and make movement easier.
- Pain Management: Ice packs, over-the-counter pain relievers, and rest help manage pain. Consult a healthcare provider for safe pain management if symptoms persist.
- Gradual Return to Normal Activities: When feeling stronger, gradually reintroduce activities rather than jumping back into strenuous tasks. This helps prevent re-injury and ensures steady progress.
Adjusting habits and following these recommendations allows individuals to cope with the limitations of an MCL injury while promoting optimal recovery.
Conclusion
Injuries to the Medial Collateral Ligament can range from minor sprains to complete tears, each requiring appropriate care and attention for full recovery. Whether through non-surgical means or surgical intervention, treating an MCL injury involves careful adherence to a tailored recovery plan, including physical therapy and rehabilitation. Taking proactive steps to strengthen the knee and prevent future injuries can ensure long-term knee health and stability. For those dealing with knee pain or suspected injuries, early diagnosis and professional guidance are essential to a safe and effective recovery.
References and External Links
- American Academy of Orthopaedic Surgeons (AAOS)
- Comprehensive information on MCL injuries, symptoms, and treatments.
- https://orthoinfo.aaos.org/
- Mayo Clinic – Knee Ligament Injuries
- Detailed explanations of MCL injuries, including causes and prevention tips.
- https://www.mayoclinic.org/
- Johns Hopkins Medicine – MCL Injury
- Offers insights into knee ligament anatomy, injury classifications, and treatment.
- https://www.hopkinsmedicine.org/
- National Institutes of Health (NIH) – Medial Collateral Ligament Injuries
- Research articles and scientific resources on MCL injury management and rehabilitation.
- https://www.ncbi.nlm.nih.gov/
- Cleveland Clinic – Medial Collateral Ligament Injury
- Covers symptoms, diagnosis, and recovery information specific to MCL injuries.
- https://my.clevelandclinic.org/
Frequently Asked Questions (FAQs)
1. How do I know if I have an MCL injury or a different knee injury?
- Symptoms like pain along the inner knee, swelling, and instability suggest an MCL injury. However, only a medical evaluation and imaging can confirm the specific injury and rule out others, like ACL or meniscus tears.
2. Can I walk with an MCL tear?
- In most cases, individuals with mild to moderate MCL injuries can still walk, though it may be painful. Using a brace and avoiding putting too much weight on the knee can help manage discomfort and promote healing.
3. Are MCL injuries common in non-athletes?
- Yes, while athletes have a higher risk, MCL injuries can occur in non-athletes due to falls, sudden knee twists, or accidents that apply force to the knee.
4. Is surgery always required for an MCL tear?
- No, most MCL injuries, especially Grades 1 and 2, heal with non-surgical treatments. Surgery is usually considered only for Grade 3 injuries or when conservative treatments don’t lead to improvement.
5. How long should I wear a knee brace after an MCL injury?
- The duration depends on the injury severity. For mild sprains, 1-2 weeks may suffice, while severe tears might require bracing for several weeks. Your doctor will provide guidance based on your recovery progress.