An article Truth Of Valvar Heart Disease exploring about the Valvar heart disease (VHD) encompasses a range of conditions that affect one or more of the heart’s valves, which regulate blood flow through the heart’s chambers. This blog explores the nature and causes of VHD, its natural history, medical management, the role of surgery, rehabilitation, and provides a comprehensive FAQ section to clarify common queries related to this condition.
Nature and Causes for Valvar Heart Disease
Stenosis and Regurgitation are mainly two types of valvar heart disease. In Stenosis, a valve becomes narrowed and hindering blood flow and in regurgitation, a valve does not close properly, and causing blood to flow backward.
Causes of Valvar Heart Disease
- Rheumatic Fever: A complication of untreated streptococcal throat infections, rheumatic fever can damage heart valves, particularly the mitral and aortic valves.
- Degenerative Changes: Aging can lead to calcification and degeneration of heart valves, commonly seen in the aortic valve, resulting in aortic stenosis.
- Congenital Heart Defects: Some individuals are born with malformed heart valves, leading to dysfunction over time.
- Infective Endocarditis: This infection of the heart lining can damage valves, leading to either regurgitation or stenosis.
- Other Medical Conditions: Conditions such as Marfan syndrome, lupus, and other connective tissue disorders can also affect heart valves.
- Lifestyle Factors: Hypertension, smoking, and hyperlipidemia contribute to the development of atherosclerosis, which can indirectly affect valvar health.
Conclusion of Nature and Causes of Valvar Heart Disease
Understanding the nature and causes of valvar heart disease is essential for early detection and management. Recognizing risk factors can help mitigate the likelihood of developing these conditions.
Natural History of Valvar Heart Disease
The natural history of valvar heart disease varies significantly based on the type and severity of the valve disorder.
Progression of Disease
- Aortic Stenosis: Often develops slowly, with symptoms appearing decades after the initial valve calcification. Patients may experience symptoms like exertional dyspnea, angina, or syncope, often leading to heart failure if left untreated.
- Mitral Regurgitation: Can be acute or chronic. Acute cases, often due to infective endocarditis or rupture of chordae tendinae, can lead to rapid deterioration. Chronic cases may remain asymptomatic for years before manifesting symptoms.
- Mitral Stenosis: Commonly results from rheumatic fever and progresses slowly. Patients may not exhibit symptoms until significant obstruction occurs.
- Pulmonary and Tricuspid Valve Diseases: Often less common and typically occur in conjunction with other cardiac conditions, making their natural history more variable.
Prognosis of Valvar Heart Disease
Prognosis depends on factors such as the specific valve affected, the severity of the dysfunction, the presence of coexisting heart disease, and patient demographics. Regular follow-up with echocardiograms and clinical evaluations is crucial in monitoring disease progression.
Medical Management for Valvar Heart Disease
The medical management of valvar heart disease focuses on symptom relief and the prevention of complications.
Pharmacological Treatments of Valvar Heart Disease
- Diuretics: Help manage fluid overload, especially in heart failure.
- Anticoagulants: Patients with mechanical valves require anticoagulation to prevent thromboembolic events.
- Beta-blockers and ACE Inhibitors: Can be beneficial in controlling heart rate and managing hypertension, respectively.
- Digoxin: Sometimes used to improve heart contractility in heart failure associated with valvar disease.
- Antibiotic Prophylaxis: Recommended for certain patients to prevent infective endocarditis during surgical procedures.
Monitoring and Follow-Up for Valvar Heart Disease
Regular monitoring is vital. Echocardiography is the primary tool for assessing the severity of valvar dysfunction, measuring changes over time, and determining when surgical intervention may be necessary.
The Role of Surgery in Valvar Heart Disease
If a cardiac surgeon feels the need of surgical intervention in a compromised heart function person so do the needful and may become necessary for patients with significant valvar heart disease who are symptomatic.
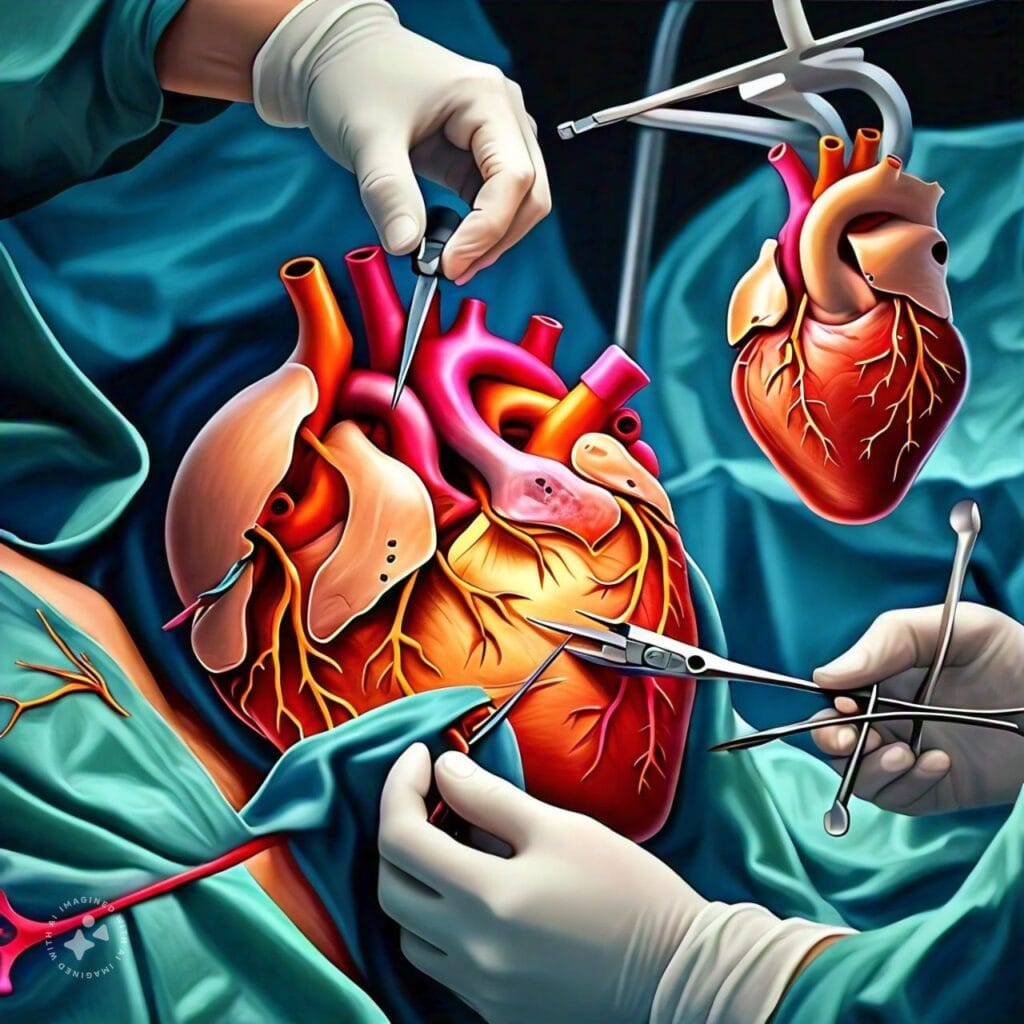
Types of Surgical Interventions
- Valvuloplasty: A procedure to repair a narrowed valve often performed on the mitral or pulmonary valve.
- Valve Replacement: Involves removing a diseased valve and replacing it with a mechanical or bioprosthetic valve. This is often indicated in severe cases of aortic stenosis or mitral regurgitation.
- Minimally Invasive Techniques: Newer approaches are available that reduce recovery time and complications associated with open-heart surgery.
Outcomes of Surgical Intervention in Valvar Heart Disease
Surgical interventions can significantly improve symptoms and quality of life. The outcomes are generally favorable, especially when performed before the onset of irreversible cardiac damage.
The Role of Rehabilitation in Valvar Heart Disease
Rehabilitation is a crucial component of the management plan for patients with valvar heart disease (VHD). It aims to enhance physical fitness, improve quality of life, and prevent future cardiac events. A structured cardiac rehabilitation program provides comprehensive support that encompasses physical, educational, and emotional aspects of recovery.
Benefits of Cardiac Rehabilitation in Valvar Heart Disease
- Improved Exercise Tolerance: Rehabilitation helps patients regain strength and stamina, enhancing their ability to engage in daily activities.
- Symptom Management: Patients often experience reduced symptoms such as fatigue and shortness of breath.
- Risk Factor Modification: Education on lifestyle changes, including diet and exercise; helps manage risk factors like hypertension and obesity.
- Psychosocial Support: Addressing mental health issues like anxiety and depression is essential, as heart disease can significantly affect emotional well-being.
- Reduced Hospital Readmission: Patients who participate in rehabilitation are less likely to be readmitted for cardiovascular complications.
Step-by-Step Guide to Cardiac Rehabilitation in Valvar Heart Disease
Step 1: Referral and Initial Assessment
- Referral: After diagnosis or post-surgery, your healthcare provider will refer you to a cardiac rehabilitation program.
- Initial Assessment: A comprehensive evaluation will be conducted, including:
- Medical history review
- Physical examination
- Assessment of functional capacity (often via a stress test)
- Evaluation of psychological well-being
Step 2: Goal Setting
- Individualized Goals: Based on the assessment, rehabilitation specialists will work with you to set specific, measurable, achievable, relevant, and time-bound (SMART) goals. These may include improving exercise capacity, managing weight, or controlling blood pressure.
Step 3: Designing the Program
- Tailored Exercise Plan: A personalized exercise regimen will be created, typically incorporating:
- Aerobic exercises (walking, cycling, swimming)
- Strength training
- Flexibility exercises
- Frequency and Duration: The program often consists of supervised sessions 2-3 times a week for 12-36 weeks, gradually increasing in intensity.
Step 4: Education and Lifestyle Modification
- Nutritional Counseling: Guidance on heart-healthy diets, including low-sodium, low fat, and high-fiber foods.
- Medication Management: Education on the importance of adhering to prescribed medications.
- Behavioral Changes: Support for smoking cessation, stress management techniques, and sleep hygiene practices.
Step 5: Monitoring and Progress Evaluation
- Regular Monitoring: For ensuring the safety, during rehabilitation sessions, heart rate, blood pressure, and overall response to exercise monitored continuously.
- Progress Evaluations: Periodic reassessments will track improvements in exercise capacity, weight, and other health metrics, adjusting the program as needed.
Step 6: Gradual Transition to Independent Exercise
- Home Exercise Plan: A home care exercise program for your progress, at home is to start as soon as possible.
- Ongoing Support: Many programs offer follow-up consultations or maintenance programs to encourage long-term adherence to exercise and lifestyle changes.
Step 7: Long-Term Lifestyle Maintenance
- Establishing Routine: Incorporate regular physical activity into your daily life, aiming for at least 150 minutes of moderate-intensity exercise weekly.
- Support Networks: Engage with support groups or community resources that promote heart-healthy living.
- Regular Check-Ups: Schedule follow-up appointments with your healthcare provider to monitor heart health and address any concerns.
Conclusion for Valvar Heart Disease
Cardiac rehabilitation plays a pivotal role in managing valvular heart disease, offering a structured approach to recovery that addresses physical, emotional, and educational needs. By following this step-by-step guide, patients can enhance their recovery process, improve their quality of life, and reduce the risk of future cardiac issues.
Valvar Heart Disease References
- Otto, C. M., & Bonow, R. O. (2013). Valvular Heart Disease: A Patient-Centered Approach. New York: McGraw-Hill.
- Nishimura, R. A., & Tajik, A. J. (2016). Valvular Heart Disease: A Clinical Approach. Elsevier.
- Braunwald, E. (2018). Heart Disease: A Textbook of Cardiovascular Medicine. Elsevier.
- Enriquez-Sarano, M., & Suri, R. M. (2016). Mitral Regurgitation. Journal of the American College of Cardiology.
- Zoghbi, W. A., et al. (2017). Recommendations for the Evaluation of the Severity of Native Valvular Regurgitation with Two-Dimensional and Doppler Echocardiography. Journal of the American Society of Echocardiography.
Valvar Heart Disease External Links
- American Heart Association – Valvular Heart Disease
- Mayo Clinic – Overview of Valvular Heart Disease
- Cleveland Clinic – Valvular Heart Disease
FAQ for Valvar Heart Disease
- What is valvular heart disease? Valvular heart disease refers to any condition that affects one or more of the heart’s valves, impacting blood flow.
- What are the common symptoms? Symptoms may include shortness of breath, fatigue, palpitations, and swelling in the legs or abdomen.
- How is valvular heart disease diagnosed? Diagnosis typically involves physical examination, echocardiography, and sometimes cardiac catheterization.
- What are the treatment options? Treatment may include medications, surgical repair or replacement of valves, and lifestyle changes.
- Can valvular heart disease be prevented? While not all cases can be prevented, managing risk factors like hypertension and avoiding rheumatic fever can help.
- What is the prognosis for patients with valvular heart disease? Prognosis varies widely based on the severity and type of valve disease, but timely intervention can improve outcomes significantly.
- What lifestyle changes can help manage valvular heart disease? Regular exercise, a heart-healthy diet, maintaining a healthy weight, and avoiding smoking can help manage the condition.
- Is surgery always necessary? Surgery is typically indicated for symptomatic patients or those with significant valve dysfunction; however, not all patients will require it.
- How often should I see my doctor if I have valvular heart disease? Regular follow-up is essential, typically every 6-12 months, depending on the severity of the disease.
- What is the role of cardiac rehabilitation? Cardiac rehabilitation supports recovery through supervised exercise, education, and lifestyle modifications post-surgery or during medical management.
